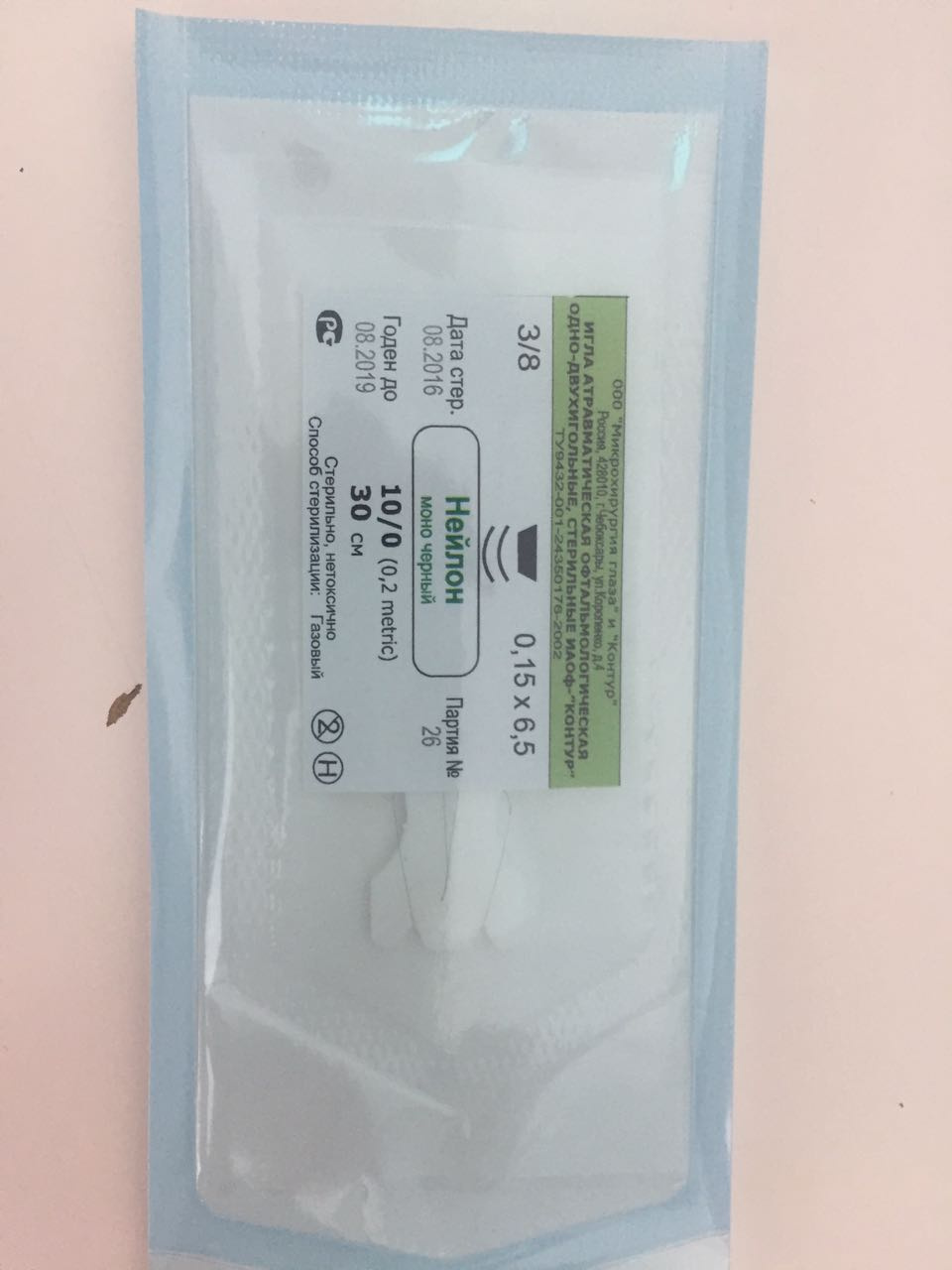
Nylon 10/0 (to sew the cornea)
For the “last chance” operation or cornea transplant, donor tissue is needed. Specifically, we are interested in tissue with a thickness of 500–600 microns for penetrating keratoplasty. Next you need to work with this film with your hands, sew with a thin nylon thread. Then, when the cornea grows together, remove the suture. No biodegradable materials — their decay products will begin to lysing and can cause inflammation, which will exclude a positive result of the operation. Moreover, the transplant is recommended to flash twice around the perimeter — this increases the chances of its correct and uniform fixation. The second layer of nylon is most often not removed at all, because as long as it does not interfere, we don’t touch it.
But let's start from the beginning. Specifically, from situations where a person may need this difficult for Russia operation, but quite familiar in Germany. It is of three types:
- PKP, that is, the removal of the entire cornea of the patient, for example, with a diameter of 7 to 8.5 mm and sewing on a new one.
- DALK, that is, corneal tissue transplantation with the exception of the Descemet's membrane and endothelium.
- DMEK, that is, the «installation» of only the layer of the Descemet's membrane and endothelial cells instead of the same layer in a patient.
Indications
DALK (Deep Anterior Lamellar Keratoplasty) is done if the upper layers of the cornea are damaged — most often keratoconus and scars, ulcers associated with accidents and other injuries that have not affected the endothelium. If the cornea has burst entirely — it is necessary to do a through, if the posterior part (endothelium layer) is preserved, try not to touch it in modern surgery. It is important that while you still have your own endothelium, which you need, because endothelial cells are not restored. This is the most difficult operation technically, and therefore quite time consuming. Well, and so dear.
DMEK (Descemet Membrane Endothelial Keratoplasty) is done with problems with the endothelium, but while maintaining the anterior layer.
Pass-throughkeratoplasty can be done in both cases, but today it is just insurance in case something went wrong during the operation or, as mentioned above, if all layers of the cornea are damaged. Most often used for ulcers with perforation.
The main indications for DMEK in Germany are genetic problems with the endothelium (for example, Fuchs dystrophy), less often the consequences of complex cataract operations when it has matured for a long time — or after a very traumatic operation. Then there are postoperative injuries, for example, after two or three operations (cataract, glaucoma, vitreoretinal intervention using silicone oil, etc.). In Russia, on the contrary, genetic factors are much less represented (perhaps because of the difference in life expectancy — in Germany, patients have time to live or be investigated), but the cataract is brought to the limit, during the removal of the lens due to the excess amount of transmitted ultrasonic energy can begin to collapse eye endothelial cells and that's it. We arrived. The corneal endothelium in humans does not multiply. At the rabbit — please.
Previously, the cornea was transplanted in a fairly simple way: the patient was cut off the layer, the layer was sewn from the donor, and waited until it was overgrown. The problem is that the larger the transplanted layer, the deeper they went into the cornea. And the deeper — the greater the volume of tissue, and the higher the chances of tissue rejection. Through keratoplasty today is used only for rare indications. In our clinic it is about 15%. For almost all other indications, minimally invasive (relatively) DMEK and DALK compete with it today, depending on which layer has suffered. It is much more difficult to do at times, but the patient has much more positive chances.
The DMEK method was developed by the Dutch doctor Gerrit Melles (by the way, like DSAEK, the method from which DMEK evolved). In our holding SMILE EYES she began to engage for the first time in 2010. So, the whole cornea is taken, and the necessary layer of 20-30 microns is separated from it. With due care, it is possible to separate in advance (for example, one hour before the operation) so that two grafts will be obtained at once — for DMEK and for DALK. Or you can order a transplant that is already prepared, but it is significantly more expensive and not always better, and any surgeon most often does it on his own. I recommend doing it yourself before the operation, because the surgeon personally controls the quality and receives fresh material. Those who perform few operations sometimes use ready-made ones (because separation is sometimes more difficult than the operation itself), but those who do not have both hands are left-handed.
The most important thing Melles came up with was not what everyone historically tried to do — sew a transplant. 150 years in a row people sewed. Dear Professor Buzin from Italy (one of my former mentors) — he tried the same thing on rabbits long before Melles, but he sewed. Did not work. And Melles said — I will inject the air bubble, and everything will suck. It was believed that he was crazy, but in fact he was a genius. It was a revolution in cornea transplantation, and it happened in a few years.
Separated film is carefully placed in the eye and pressed down with an air bubble so as not to leave. Here is a DMEK video, roughly giving a presentation:
What is important for this operation: the patient is highly recommended to be under anesthesia (to sleep and be immobilized) in order not to twitch. Under local anesthesia without tranquilizers, when a person is under tension in the eye, pressure rises, and this leaves less space in the anterior chamber of the eye for non-traumatic transplant manipulations. And the probability of hemorrhage under local anesthesia is higher. Especially important is good anesthesia for end-to-end transplants. And then, if the patient coughs during a through-transplant, we lose an eye.
In the video, the patient does not sleep, because the next anesthesia may well be the last in her life for medical reasons (does not tolerate). I operate it under local anesthesia, which somewhat increases the complexity of the operation.
The DMEK operation (on video) is performed without direct contact of the endothelial cells — the layer moves with an air bubble.
Operations on the outer layers (DALK) are made with a thin hand tool with direct touch.
Complications
Each operation is a lottery for tissue survival. In part, you can predict the chances of success on the quality of the donor product. Corneal banks consider cells and know their freshness, but vital quality cannot be predicted. That is, the cells can be «turned on», but their functionality is almost exhausted — maybe their resource will end in 2 months. As a result, transplantation in one patient allows seeing 10 years well, and in another — only a couple of years.
In second place is the work of the surgeon. It is incredibly easy to make mistakes here, so no one ever promises a “clean” DALK. One layer of cells can break from anything — from the surgeon's wrong movement, from the patient's breathing, from the fact that something has changed in the eye, and so on. Yes, there are methods that reduce the likelihood, but still there is a risk of errors, and in the course of the play, you can switch to end-to-end keratoplasty if something goes wrong.
Equipment from a certain moment almost does not affect — the operation depends entirely on skill. The cornea can also be operated with a laser at the first stage (removed by it), but the femtosecond laser has not yet shown significant results in comparison with traditional methods. There are minimal differences, but they are so small that it makes no sense to lengthen the operation (the laser increases the operation from 40 minutes to 70 minutes if the laser, for example, is in another operating room). Access is often done by hand, with good vacuum trepanning systems.
DMEK is almost always obtained from a trained surgeon, and my colleagues have never had a case of switching to a pass-through with DMEK.
Risks are strongly influenced by the condition of the patient, in particular, his age. And the most unpleasant thing is vascularization of the cornea, the very blood vessels that sprout into the cornea as a result of lack of proper access of oxygen (most often from contact lenses, as well as after burns and infections). Sharply increases the likelihood of rejection. If the cornea is without vessels, then the immune system does not have direct access to the upper layer, all immune processes proceed slowly and gently. As soon as blood (vessels) appears, the immune system begins to react very sharply to the transplant. Therefore, they first try to remove the vessels in such cases, and they are removed by laser or direct cauterization, or by special injections of growth inhibitors.
Further, there is a risk of infection. It is predictable, and it can be stopped very much, especially if you lead a quiet lifestyle.
Recovery
The eye is kept under a protective bandage for 1 day.
In the case of DMEK, a gas bubble remains in the beginning in the anterior chamber of the eye. A patient from 5 days to two weeks sees almost nothing with the operated eye, only changes in the level of illumination. From about the third of the week, the picture becomes clear, and after a month already good vision is available. The longest, in the case of running states of Fuchs dystrophy — you can not see a month.
According to our research, in 8% of cases you need to inject the second bubble — if the transplanted layer suddenly begins to move away. The need to do this is determined on inspections after surgery.
As the DALK heals and penetrates keratoplasty (but not after DMEK), the incision of the postoperative wound can be a complication. For example, the patient may fight with someone and get a fist in the eye. Older people lack a very small injury to the connection snapped.
Nylon or mercyline (10/0 threads) are removed like this: in six months the first layer, and the second — up to 3-5 years, depending on the degree of engraftment. In older people, the second layer is often not removed at all, if it does not create problems, as long as the thread is well stretched, it does not interfere. It happens that the second thread is pulled out — and the vision drops, because this thread was the skeleton of the graft, and this induces astigmatism.
After end-to-end surgery or DALK, astigmatism often appears: because even if you sew very well, scars will depend on healing. The cornea does not engraft 360 degrees evenly. In two years, it is possible to do PRK, LASIK or ReLEx SMILE right inside the transplant (I did not do the last one myself, but my colleagues from the University of Alexandria did this already). Another elegant approach to the problem of astigmatism is to change the lens to a new one if cataracts have not been treated yet. If the cataract was operated, then put a toric backpack lens (Add-on) to an artificial lens — a lens in front of the primary lens in the capsular bag. If your own lens is still transparent, the patient is young, and surgery to remove the lens is not needed, then you can put the toric ICL.
What else you need to know about keratoplasty operations in Russia
Donor material in Russia is a pain. It comes in most cases with difficulty, long and expensive. Nevertheless, there are options, just the price is far from being the same as in Europe. It was a great success that canned material appeared in an eye bank in Russia, and people got a chance for recovery. There are very few doctors who can do layered transplants. Dozens of surgeons can do the cross-cutting, the benefit of manual surgeons with good skills is many, and both in the European part of the country and in the east.