Imagine the situation — you live in peace, nothing hurts and does not blush, wear glasses or lenses, or do not use anything and see perfectly — and you accidentally get an appointment with an ophthalmologist. For example, because of conscription into the army, because of pregnancy, or just for a dispensary examination. And suddenly you will find out that your retina is “full of holes” or stretched and is about to break.
And they recommend you to “sew it on”. And you doubt — and this is exactly what you need? And how safe is it? But nothing bothers — then why? Or maybe they want to earn money on me? And the first thing you start is to read posts on the Internet, what a “independent” expert like Google will say.
And in the future everything depends on your discipline and attention to your own health. You can get to the ophthalmologist-laser specialist, who will be the last resort, and he will do preventive laser coagulation.
Or «forget it» for everything and continue to live as before — nothing bothers you. What is the risk?

To understand what works and how, we need knowledge of the anatomy of the eye.
The retina (retina) of the eye is the inner membrane, therefore, to inspect it, you need to look into the eye cavity through the pupil. The wider the pupil, the more the surface of the retina will be able to see the ophthalmologist. Therefore, to examine the fundus in the maximum amount, you need to bury the drops that can cause cycloplegia — a condition where the pupil is wide and does not respond to light. This reversible state, albeit a rather unpleasant one, passes in a couple of hours, but it makes it possible to look into the most “secret” zones of the retina.
The human retina consists of two parts.
The back is photosensitive; front end — not sensitive to light. Conventionally, the separation takes place «at the equator»: the department after the equator is the visual, or functionally active part of the retina, the neuronal retina, which we see. We don’t see a department around the equator, and problems arise there.
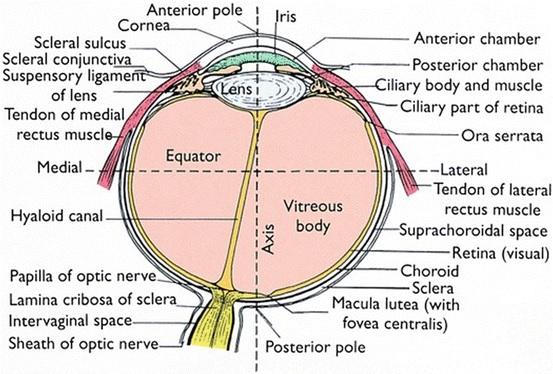
The visual part of the retina is its posterior, or photosensitive, section, a complex structure containing at least 15 types of neurons connected to each other by intercellular connections with well-developed microvilli and closure belts. These specialized compounds provide the difference in electrical potential due to the transport of ions between the surfaces. Through the intermediate layer, including conductor neurons, these cells send processes to the brain. These processes converge in the papilla of the optic nerve, forming the optic nerve.
But since none of these types of outgrowths are anatomically connected with photoreceptors, these areas can easily be separated from each other, for example, when retinal detachment develops.
If a person has a problem in the visual part, he has complaints of reduced vision, is plagued by all sorts of unpleasant symptoms such as flashes, distortions, etc.
And if the problems are in the «blind» zone, then there will be no complaints. Peripheral retinal dystrophy — an invisible danger.
The peripheral zone of the retina is practically invisible with the usual standard examination of the fundus without pupil dilation and inspection with special lenses that increase the angle and area of the review. But it is precisely at the periphery of the retina that dystrophic (degenerative) processes often develop, which are dangerous because they can lead to tears and retinal detachment. Changes in the periphery of the fundus — peripheral dystrophies of the retina — can occur in both short-sighted and far-sighted people, and in persons with normal vision.
This common and serious human disease can be effectively treated using laser surgery.
The causes of peripheral dystrophic changes in the retina are not fully understood.
Dystrophy may occur at any age, with the same probability in men and women.
There are many predisposing factors — this is myopia, regardless of the degree of minus, heredity, inflammatory diseases and eye injuries, head injuries and, of course, age.
Common diseases also have an effect: hypertension, atherosclerosis, diabetes, past infections and intoxications.
Approximately it happens this way: on the periphery of the retina, for some reason, nutrition is deteriorating, the vessels empty, this leads to metabolic depletion and thinning of local functionally modified areas.
Under the action of physical exertion, falls, conditions associated with lifting to a height or underwater immersion, acceleration, jerks and weight transfer, vibration, dystrophic altered areas can cause ruptures.
However, it has been proven that in people with myopia, peripheral degenerative changes in the retina occur much more frequently, because with myopia, the length of the eye increases, resulting in stretching of its membranes and thinning of the retina in the periphery.
The first is the size and localization. They can be multiple or single, small or huge, occupy a local zone or be located around the entire circumference of the fundus.
The second, important, is what structures of the eye are affected. Peripheral retinal dystrophy is divided into peripheral chorioretinal (PCRD), when only the retina and choroid are affected, and peripheral vitreorecorioretinal dystrophy (PWHT) — with involvement in the degenerative process of the vitreous body. What is the vitreous body and what is happening in it is described here: “Flying midges” and “glassy worms” in the eyes, or where do “broken pixels” in the vitreous body come from.
The type of dystrophy without participation of the vitreous is more benign. Such options include, for example, dystrophy of the type “cobblestone pavement”.
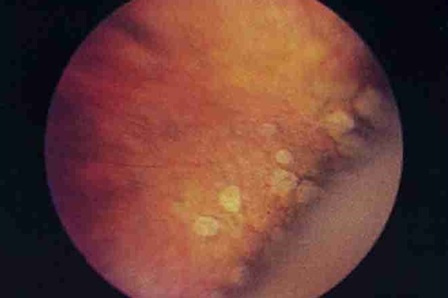
Type of dystrophy «cobblestone pavement»
If in the dystrophy zone there are adhesions with the vitreous body, then often tractions (cords, adhesions) form between the modified vitreous body and the retina. It is highly likely that for any deformity it will pull the retina behind itself into the eye. Such adhesions, joining one end to the thinned area of the retina, many times increase the risk of ruptures and subsequent detachment. And this is all the chances of losing sight or degrading the optical quality of the eye to a few percent of the norm.
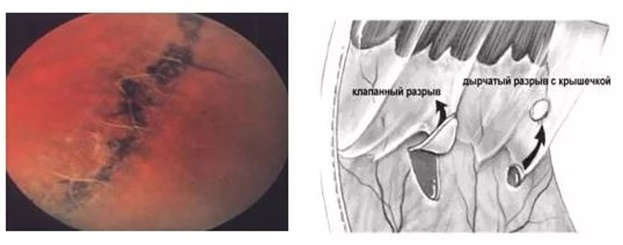
Dystrophy type «lattice dystrophy» and retinal breaks
Such tears and dystrophies occur imperceptibly for the patient and are found not only in the near-sighted, but also in the far-sighted, and in people with absolutely normal optics of the eye.
In myopic people, as a rule, the axial length of the eye is more than 24 mm (the average parameter, the measurement of which tells us about the progression of myopia). There is a risk that the eye, increasing (and an increase in the eye — this is, in fact, myopia) begins to pull the vitreous body (because the rest of the tissues stretch very little). Dystrophic chorioretinal processes on the periphery of the retina (“lattice degeneration”, “snail track”, etc.) lead to thinning of the retina and its ruptures.
With them, one can live as a whole without any symptoms, but the risk of retinal detachment in these cases is very high.
Peripheral dystrophies are asymptomatic and dangerous. Sometimes patients come with complaints of floating cloud and midges before the eyes, less likely to be disturbed by «sparks» and «lightning» at the periphery. That is, the symptoms are rare and scanty.
And then it all depends on the ophthalmologist — will he persuade you to expand the pupil and see how the retina should be? Can you see problems and interprets what you see correctly? Whether it is enough to equip an office for diagnostics — it will simply not be possible to see with an ophthalmoscope flashlight, you need special lenses (contact or contactless). Is there a necessary diode laser in the clinic or will it be necessary to run and search for a clinic and a specialist who will strengthen the retina?
Full diagnostics of peripheral dystrophy and “silent” tears (without retinal detachment) is possible when examining the fundus in conditions of maximum medical expansion of the pupil using a special lens, which allows you to view the most “remote” areas of the retina to the equator. If necessary, you can even use sclerocompression — indentation of the sclera as if inside the eyeball, thus the retina is shifted from the periphery to the center, with the result that some peripheral areas inaccessible for inspection become visible. This is all done after instillation of a local anesthetic for superficial freezing of the eye. The procedure will worsen your near vision somewhat, photophobia will increase by a couple of hours, but all these symptoms always pass on average in a couple of hours. So do not refuse it at all!
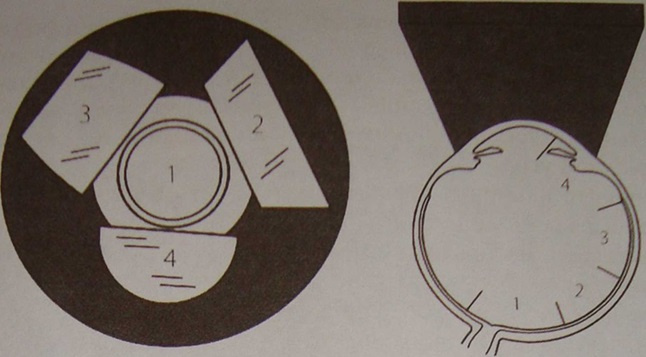
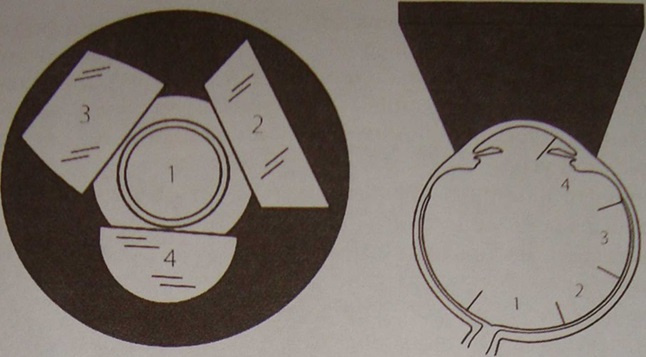
By the way, for inspection, you need to use not a flashlight, as is done in most clinics, but special lenses for examining the fundus. There is a universal contact lens — Goldman's lens. This flat lens with a system of three mirrors is very widely used in the examination and laser coagulation of the anterior segment of the eye and retina.

Goldman's three-mirror lens
In each mirror, we see different parts of the retina, and, turning it clockwise, we get complete information. Something like this:
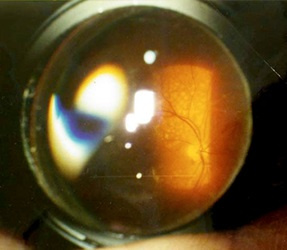
And this is the scheme in which mirror which department of the eye we inspect:
To date, there are also special digital cameras with which you can get a color image of the periphery of the retina in the presence of dystrophy and rupture zones.
Well, and most importantly — the ophthalmologist must not only pretend that he is looking at the lens, he must be able to see and interpret what he has seen. My experience in treating detachments and problems with the vitreous body and retina indicates a sad situation.
In half of the clinics sit doctors who do not even dilate the pupil for examination. Half of the remaining half looks with a direct ophthalmoscope — it shines a flashlight into the eye, while at best it sees only the center. The next half of the remaining quarter has lenses and looks, but does not understand anything in what they see!
So, only 10-15% of patients receive high-quality diagnostics! The remaining 85-90% of doctors rely on luck, or refer to the fact that they do not have the necessary equipment.
The main necessary «equipment» for the diagnosis — the doctor's eyes and his professional intelligence.
The source of radiation in coagulation lasers is a diode-pumped solid-state laser.
The goal of this treatment is to prevent retinal detachment.
Perform preventive barrier coagulation of the retina in the field of dystrophic changes or border laser coagulation around an existing gap. An impact on the retina along the edge of a dystrophic focus or rupture is performed, resulting in a “gluing” of the retina to the underlying eye shells at the points of exposure to laser radiation. Let me remind you that we are talking about those areas of the retina with which we «do not see», therefore after this procedure and the narrowing of the pupil, the vision is completely restored to the original.
The procedure is performed with a Goldman contact lens on the eye. This prevents involuntary eye movements and allows you to accurately focus the laser beam on the problem area.
The patient senses the laser action as flashes of bright light. As a rule, they do not cause any discomfort, but sometimes there may be a slight tingling, dizziness, or even nausea. The operation takes place in a sitting position. The eye itself is securely fixed, and the beam on a healthy retina is excluded.
Laser coagulation is performed on an outpatient basis and is well tolerated by patients. It is necessary to take into account that the process of formation of adhesions takes some time, therefore, after laser coagulation is carried out, it is recommended to avoid large physical exertion, such as parachute jumping, weight lifting, etc. within 10-14 days. Otherwise, you can lead a normal life and drip 3-4 times a day preventive drops.

Diagram of coagulation dystrophy zone with a gap
During pregnancy, it is necessary to inspect the fundus of the eye on the wide pupil at least twice — at the beginning and at the end of pregnancy. After delivery, an ophthalmologist examination is also recommended.
If there is a problem, then in terms of up to 36 weeks we are quite calmly performing laser coagulation of the retina. Although, the sooner it is found, the better. Since in the last months to sit during this procedure is not very convenient. After 36-37 weeks, we believe that it is too late to coagulate — spikes may simply not have time to form.
Delimited zones of dystrophy, adhesions and tears are not a contraindication to natural childbirth, of course, if there are no obstetric contraindications.
Prevention of the dystrophic processes themselves on the periphery of the retina is possible in representatives of the risk group — these are myopic, patients with hereditary predisposition, children born after a severe course of pregnancy and childbirth, patients with hypertension, diabetes, vasculitis and other diseases for which deterioration of peripheral circulation is observed. Such people are also recommended regular preventive examinations by an ophthalmologist with an examination of the fundus.
In itself, the presence of dystrophy at the periphery is not a contraindication for laser vision correction. Preventive laser “stitching” is done on medical advances, regardless of whether there will be a subsequent correction or not.
For LASIK, the retina is pre-strengthened, since the vacuum ring significantly increases the pressure, increasing the risk of retinal detachment.
For methods such as SMILE or FemtoLASIK, it is not so important when preventive peripheral laser coagulation of the retina (PPLK) is performed — before or after correction, as there is no increase in intraocular pressure.

And they recommend you to “sew it on”. And you doubt — and this is exactly what you need? And how safe is it? But nothing bothers — then why? Or maybe they want to earn money on me? And the first thing you start is to read posts on the Internet, what a “independent” expert like Google will say.
And in the future everything depends on your discipline and attention to your own health. You can get to the ophthalmologist-laser specialist, who will be the last resort, and he will do preventive laser coagulation.
Or «forget it» for everything and continue to live as before — nothing bothers you. What is the risk?
To understand what works and how, we need knowledge of the anatomy of the eye.
The retina (retina) of the eye is the inner membrane, therefore, to inspect it, you need to look into the eye cavity through the pupil. The wider the pupil, the more the surface of the retina will be able to see the ophthalmologist. Therefore, to examine the fundus in the maximum amount, you need to bury the drops that can cause cycloplegia — a condition where the pupil is wide and does not respond to light. This reversible state, albeit a rather unpleasant one, passes in a couple of hours, but it makes it possible to look into the most “secret” zones of the retina.
The human retina consists of two parts.
The back is photosensitive; front end — not sensitive to light. Conventionally, the separation takes place «at the equator»: the department after the equator is the visual, or functionally active part of the retina, the neuronal retina, which we see. We don’t see a department around the equator, and problems arise there.
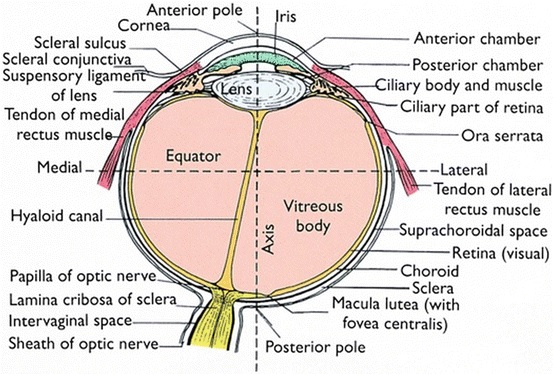
The visual part of the retina is its posterior, or photosensitive, section, a complex structure containing at least 15 types of neurons connected to each other by intercellular connections with well-developed microvilli and closure belts. These specialized compounds provide the difference in electrical potential due to the transport of ions between the surfaces. Through the intermediate layer, including conductor neurons, these cells send processes to the brain. These processes converge in the papilla of the optic nerve, forming the optic nerve.
But since none of these types of outgrowths are anatomically connected with photoreceptors, these areas can easily be separated from each other, for example, when retinal detachment develops.
Independently it is possible to detect the peripheral distrophy of the retina?
If a person has a problem in the visual part, he has complaints of reduced vision, is plagued by all sorts of unpleasant symptoms such as flashes, distortions, etc.
And if the problems are in the «blind» zone, then there will be no complaints. Peripheral retinal dystrophy — an invisible danger.
The peripheral zone of the retina is practically invisible with the usual standard examination of the fundus without pupil dilation and inspection with special lenses that increase the angle and area of the review. But it is precisely at the periphery of the retina that dystrophic (degenerative) processes often develop, which are dangerous because they can lead to tears and retinal detachment. Changes in the periphery of the fundus — peripheral dystrophies of the retina — can occur in both short-sighted and far-sighted people, and in persons with normal vision.
This common and serious human disease can be effectively treated using laser surgery.
Possible causes of dystrophy in grindle periphery
The causes of peripheral dystrophic changes in the retina are not fully understood.
Dystrophy may occur at any age, with the same probability in men and women.
There are many predisposing factors — this is myopia, regardless of the degree of minus, heredity, inflammatory diseases and eye injuries, head injuries and, of course, age.
Common diseases also have an effect: hypertension, atherosclerosis, diabetes, past infections and intoxications.
Approximately it happens this way: on the periphery of the retina, for some reason, nutrition is deteriorating, the vessels empty, this leads to metabolic depletion and thinning of local functionally modified areas.
Under the action of physical exertion, falls, conditions associated with lifting to a height or underwater immersion, acceleration, jerks and weight transfer, vibration, dystrophic altered areas can cause ruptures.
However, it has been proven that in people with myopia, peripheral degenerative changes in the retina occur much more frequently, because with myopia, the length of the eye increases, resulting in stretching of its membranes and thinning of the retina in the periphery.
What is the difference between distrophy
The first is the size and localization. They can be multiple or single, small or huge, occupy a local zone or be located around the entire circumference of the fundus.
The second, important, is what structures of the eye are affected. Peripheral retinal dystrophy is divided into peripheral chorioretinal (PCRD), when only the retina and choroid are affected, and peripheral vitreorecorioretinal dystrophy (PWHT) — with involvement in the degenerative process of the vitreous body. What is the vitreous body and what is happening in it is described here: “Flying midges” and “glassy worms” in the eyes, or where do “broken pixels” in the vitreous body come from.
The type of dystrophy without participation of the vitreous is more benign. Such options include, for example, dystrophy of the type “cobblestone pavement”.
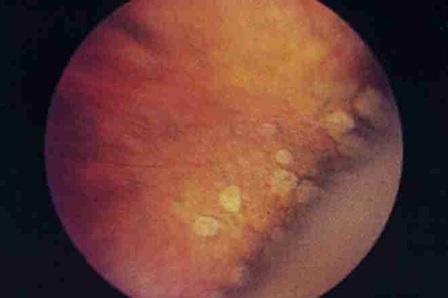
Type of dystrophy «cobblestone pavement»
If in the dystrophy zone there are adhesions with the vitreous body, then often tractions (cords, adhesions) form between the modified vitreous body and the retina. It is highly likely that for any deformity it will pull the retina behind itself into the eye. Such adhesions, joining one end to the thinned area of the retina, many times increase the risk of ruptures and subsequent detachment. And this is all the chances of losing sight or degrading the optical quality of the eye to a few percent of the norm.
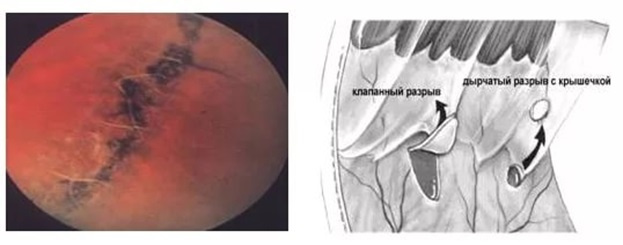
Dystrophy type «lattice dystrophy» and retinal breaks
Such tears and dystrophies occur imperceptibly for the patient and are found not only in the near-sighted, but also in the far-sighted, and in people with absolutely normal optics of the eye.
What is happening with a close?
In myopic people, as a rule, the axial length of the eye is more than 24 mm (the average parameter, the measurement of which tells us about the progression of myopia). There is a risk that the eye, increasing (and an increase in the eye — this is, in fact, myopia) begins to pull the vitreous body (because the rest of the tissues stretch very little). Dystrophic chorioretinal processes on the periphery of the retina (“lattice degeneration”, “snail track”, etc.) lead to thinning of the retina and its ruptures.
With them, one can live as a whole without any symptoms, but the risk of retinal detachment in these cases is very high.
Diagnostics of peripheral dystrophy and retractable gaps
Peripheral dystrophies are asymptomatic and dangerous. Sometimes patients come with complaints of floating cloud and midges before the eyes, less likely to be disturbed by «sparks» and «lightning» at the periphery. That is, the symptoms are rare and scanty.
And then it all depends on the ophthalmologist — will he persuade you to expand the pupil and see how the retina should be? Can you see problems and interprets what you see correctly? Whether it is enough to equip an office for diagnostics — it will simply not be possible to see with an ophthalmoscope flashlight, you need special lenses (contact or contactless). Is there a necessary diode laser in the clinic or will it be necessary to run and search for a clinic and a specialist who will strengthen the retina?
Full diagnostics of peripheral dystrophy and “silent” tears (without retinal detachment) is possible when examining the fundus in conditions of maximum medical expansion of the pupil using a special lens, which allows you to view the most “remote” areas of the retina to the equator. If necessary, you can even use sclerocompression — indentation of the sclera as if inside the eyeball, thus the retina is shifted from the periphery to the center, with the result that some peripheral areas inaccessible for inspection become visible. This is all done after instillation of a local anesthetic for superficial freezing of the eye. The procedure will worsen your near vision somewhat, photophobia will increase by a couple of hours, but all these symptoms always pass on average in a couple of hours. So do not refuse it at all!
By the way, for inspection, you need to use not a flashlight, as is done in most clinics, but special lenses for examining the fundus. There is a universal contact lens — Goldman's lens. This flat lens with a system of three mirrors is very widely used in the examination and laser coagulation of the anterior segment of the eye and retina.

Goldman's three-mirror lens
In each mirror, we see different parts of the retina, and, turning it clockwise, we get complete information. Something like this:
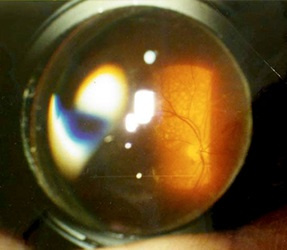
And this is the scheme in which mirror which department of the eye we inspect:
To date, there are also special digital cameras with which you can get a color image of the periphery of the retina in the presence of dystrophy and rupture zones.
Well, and most importantly — the ophthalmologist must not only pretend that he is looking at the lens, he must be able to see and interpret what he has seen. My experience in treating detachments and problems with the vitreous body and retina indicates a sad situation.
In half of the clinics sit doctors who do not even dilate the pupil for examination. Half of the remaining half looks with a direct ophthalmoscope — it shines a flashlight into the eye, while at best it sees only the center. The next half of the remaining quarter has lenses and looks, but does not understand anything in what they see!
So, only 10-15% of patients receive high-quality diagnostics! The remaining 85-90% of doctors rely on luck, or refer to the fact that they do not have the necessary equipment.
The main necessary «equipment» for the diagnosis — the doctor's eyes and his professional intelligence.
Lasercoagulation of peripheral distrophy and zinary return zones
The source of radiation in coagulation lasers is a diode-pumped solid-state laser.
The goal of this treatment is to prevent retinal detachment.
Perform preventive barrier coagulation of the retina in the field of dystrophic changes or border laser coagulation around an existing gap. An impact on the retina along the edge of a dystrophic focus or rupture is performed, resulting in a “gluing” of the retina to the underlying eye shells at the points of exposure to laser radiation. Let me remind you that we are talking about those areas of the retina with which we «do not see», therefore after this procedure and the narrowing of the pupil, the vision is completely restored to the original.
The procedure is performed with a Goldman contact lens on the eye. This prevents involuntary eye movements and allows you to accurately focus the laser beam on the problem area.
The patient senses the laser action as flashes of bright light. As a rule, they do not cause any discomfort, but sometimes there may be a slight tingling, dizziness, or even nausea. The operation takes place in a sitting position. The eye itself is securely fixed, and the beam on a healthy retina is excluded.
Laser coagulation is performed on an outpatient basis and is well tolerated by patients. It is necessary to take into account that the process of formation of adhesions takes some time, therefore, after laser coagulation is carried out, it is recommended to avoid large physical exertion, such as parachute jumping, weight lifting, etc. within 10-14 days. Otherwise, you can lead a normal life and drip 3-4 times a day preventive drops.
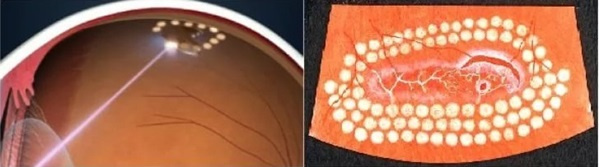
Diagram of coagulation dystrophy zone with a gap
How about pregnancy and childbirth
During pregnancy, it is necessary to inspect the fundus of the eye on the wide pupil at least twice — at the beginning and at the end of pregnancy. After delivery, an ophthalmologist examination is also recommended.
If there is a problem, then in terms of up to 36 weeks we are quite calmly performing laser coagulation of the retina. Although, the sooner it is found, the better. Since in the last months to sit during this procedure is not very convenient. After 36-37 weeks, we believe that it is too late to coagulate — spikes may simply not have time to form.
Delimited zones of dystrophy, adhesions and tears are not a contraindication to natural childbirth, of course, if there are no obstetric contraindications.
Prevention of the dystrophic processes themselves on the periphery of the retina is possible in representatives of the risk group — these are myopic, patients with hereditary predisposition, children born after a severe course of pregnancy and childbirth, patients with hypertension, diabetes, vasculitis and other diseases for which deterioration of peripheral circulation is observed. Such people are also recommended regular preventive examinations by an ophthalmologist with an examination of the fundus.
Peripheral distrophies of the retail and laser view correction
In itself, the presence of dystrophy at the periphery is not a contraindication for laser vision correction. Preventive laser “stitching” is done on medical advances, regardless of whether there will be a subsequent correction or not.
For LASIK, the retina is pre-strengthened, since the vacuum ring significantly increases the pressure, increasing the risk of retinal detachment.
For methods such as SMILE or FemtoLASIK, it is not so important when preventive peripheral laser coagulation of the retina (PPLK) is performed — before or after correction, as there is no increase in intraocular pressure.

Tips from me personally
- Never refuse to check the fundus with the expansion of the pupil for your own safety. Most often, retinal dystrophies are found by chance.
- If there are complaints about the occurrence of lightning, flashes, the sudden appearance of more or less number of floating flies go immediately to the reception of an ophthalmologist, this may indicate already existing retinal breakdown.
- Do not refuse to examine the periphery with the help of the Goldman contact lens — this will allow you to see the most extreme areas of the retina.
- You can fix the presence of problem areas on special digital equipment and evaluate them in relation to the entire fundus area. Serious clinics have this capability and equipment.
- When peripheral dystrophy and retinal tears are detected, laser treatment is performed to prevent retinal detachment, so the sooner you do this procedure, the better.
- The main way to prevent these complications is the timely diagnosis of peripheral retinal dystrophy in patients at risk, followed by regular monitoring and, if necessary, preventive laser coagulation.
- Patients with existing pathology of the retina and patients at risk should undergo an examination 1 — 2 times a year.
- Do not deprive the opportunity of your child to be born naturally — do timely preventive examinations during pregnancy and laser coagulation according to indications.