Now I will show what doctors usually never show to patients. More precisely, it shows everything in the form of a beautiful render, from which it does not follow at all that a piece of metal will stick up in your cornea for a couple of minutes. Fortunately, you will not feel this because of the anesthetic premedication, you will not know and do not remember, because the piece of iron will be out of focus.

So, watch the video, and I will show the frames with comments. This is a real operation on a patient in a German clinic, the recording was made on a device like the “black box” of the VisuMAX device. In this case, the patient has agreed to use the recording for training purposes, usually access to such records is strictly limited.
First, briefly repeat the last post about why you need to cut just such a lens inside the eye, and then get it:
Very briefly, the operations of past generations formed just such an unpleasant “lid” that kept on one flap during healing. The “cover” of the flap is removed, the lens is evaporated, the “cover” is put back.
The invasiveness is high, the “lid” never takes root completely (with injuries and physical exertion it sometimes comes off with extremely unpleasant consequences), a lot of heat is used in the incisions that penetrates into the eye tissues, the Bowman's membrane is severely damaged both by cutting and by thermal fronts.
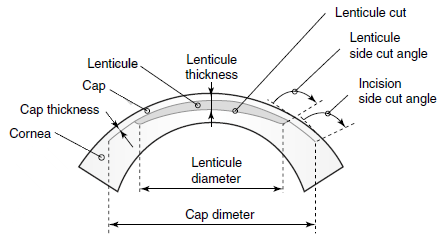
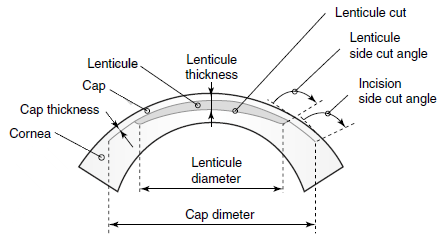
The idea of the next generation is to cut the lens right inside the cornea, and then get it through a thin incision without this “cap”. The effect is possible because lasers allow focusing inside the tissue, not on its surface. That is, you can make a cut here according to this scheme:
Now we are watching the render operation:
First, the bottom surface of the lens inside the cornea, then the top, then a small incision on the side — and remove the lens with tweezers.
This is what any clinic will show you so that you do not get scared. The real operation looks like this (now telemetry):
First, the patient is asked to look at the flashing green light. The lamp does not just burn, but flashes, so that a person catches it in focus quite often. The eye makes an incredible amount of micro movements, saccades per second, but this is the pace that allows the surgeon to produce a proper eye grip later.

Here you can see the tampon in the defocus (in the video it moves on the left side of the eye) — this surgeon once again wipes the surface to insure against the microbunches of fat floating on it. The second purpose of this touch is to check how the premedication went. The patient must answer if he senses something. He should not feel anything, his nerves are already disconnected with tetracaine.

Here is the capture approaching the eye, which is clearly seen by the appearance closer to the zone of sharpness of the iris:

Alignment and fixation of pneumatic grip is performed. The moment of capture itself can be seen by an easy rotation of the eye, and this effect is very important to control during the correction of astigmatism, because a turn of 30 degrees negates the whole operation for the case of astigmatism. Therefore, the surgeon adjusts the alignment.

After a successful capture, we switch the observation range from visible to infrared to control the process and not blind the patient:

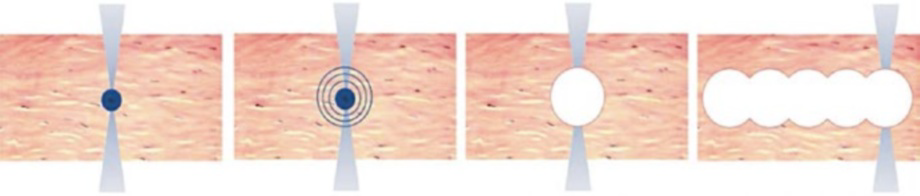
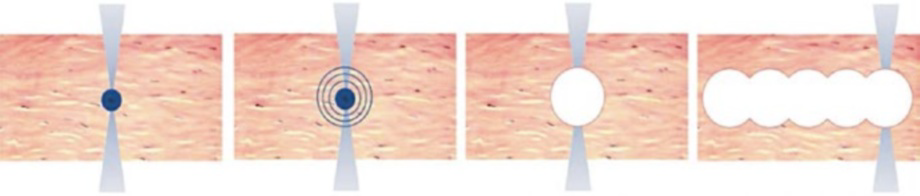
Slowly expanding ring from the edges of the eye to the center is the millions of femtolaser micropulses that form a cut on the upper surface of the lenticular lens inside the cornea. The surface of the cornea is not cut. I recall the main effect — the evaporation of several cells inside the layer of the cornea, and then the release of a relatively large amount of gas, gently pushing tissue.

The bottom surface of the lens is finished:

The second circle, which expands from the center of the eye to the edges, is the upper surface of the lens, which is also cut inside the cornea layer, without direct “piercing” the surface:

At about 01:02 a cut is formed through the surface of the cornea to the cut lens. Lenticule, but in the video it is extremely difficult to make out. Through this incision the lens will reach.
Now, switching the view (and the end of the video from the laser) — the patient from under the control of the CNC is given under the hands of the surgeon (in fact, he moves under the device from under the laser closer to the doctor’s hands). The first step is to wet the eye:

Switching the lens of the microscope, fixing the eye so that it does not twitch, with tweezers. It tucks, but the patient did not feel (for pain relief) and does not even see the tweezers properly (or rather, sees the surgeon's hands above his head):

The incision to extract lentikuly neatly divided instrument — spatula:

This is a very interesting place, the first small spatula First, the upper edge of the lens and the surrounding tissues are separated, and then the lower edge of the lens (in the frame below):

The spatula moves with inconspicuous jerks — this is the resistance of the micro-spikes, arising from the discrete structure of the cut, in some places the individual fibers are not “unstick”, and they need to be moved apart. It’s just not possible to pull the lenticule over the edge, it can catch, so a full spatula is always made on the surface so that air enters the cavity between the upper edge of the lens and the cornea and the lower edge of the lens and the cornea. The most terrible part is as follows:

The surgeon’s hand lies with his elbow on a special support, and with his wrist rests on the patient’s forehead. The spatula is designed so that even if the surgeon is pushed (slightly) or the patient is distracted by a loud bang, the eye will not be damaged. However, all such factors should be strictly excluded.
So, the lens is divided and ready for extraction from the inside of the cornea. The surgeon picks up the tweezers and catches the lenticle:



That's it. You can finish this, but you still need to wash the eyes. Here you can see how the supply of fluid works:

The next stage is the supply of saline directly into the cavity inside the cornea:

As you can see, it will later flow out through the same incision through which the lenticule has been removed. Previously, a second incision was made opposite the first (at the other pole of the eye) to remove this fluid, but it turned out that there was no need for this. Moreover, the smaller the cut, the better.
Smoothing to avoid micro-tabs:

Then — removal of fixing films and the final. You can blink a couple of times. The patient rests for a few seconds, and then slowly gets up and walks into the corridor. In each clinic at the end of the corridor there are hours for control. Next is the dialogue to calm the worrying patient:
“What time is it there?”
— Six minutes past eleven.
— And would you have distinguished the clock from such a distance?
— Oh. For sure.
— Well, everything is in order.
The patient calms down and goes to rest. After 2-3 hours, the eye does not feel anything. You cannot read, write, use a phone or tablet laptop for a day or two to promote fast healing (after all, reading is jogging for the eyes, then you cannot go to a hard sauna or swimming pool for two weeks (until the incision is completely healed to remove lenticules). did not get an infection). That's all.
I hope you have not run away in horror when you saw the spatula. Despite the frightening, I note that this is one of the easiest operations. Gathering the eyes piece by piece after an accident with taking out glass fragments and other side charms on a few hours l bo most precise manual work mikroskalpelem much more difficult and stressful.
On questions of exactly how pneumatic grip works, how you can precisely cut the lens of the desired shape and diameter, what happens to the cornea tissues at the cut border, and why are there such difficulties with cutting the lens inside the eye (and why it is safest). Plus, how the operating room is prepared, how the surgeon soothes the patient, how premedication is performed, what kind of protection there is against unforeseen situations (interruptions in food passing a truck), and so on, I will answer with the next big post. And about the promised comparison of lenses and operations, too, later. All this is a separate topic for discussion, and about them a little later, alas, does not come out much to write. In the first post in the discussion, many topics are superficially affected.

So, watch the video, and I will show the frames with comments. This is a real operation on a patient in a German clinic, the recording was made on a device like the “black box” of the VisuMAX device. In this case, the patient has agreed to use the recording for training purposes, usually access to such records is strictly limited.
First, briefly repeat the last post about why you need to cut just such a lens inside the eye, and then get it:
Very briefly, the operations of past generations formed just such an unpleasant “lid” that kept on one flap during healing. The “cover” of the flap is removed, the lens is evaporated, the “cover” is put back.
The invasiveness is high, the “lid” never takes root completely (with injuries and physical exertion it sometimes comes off with extremely unpleasant consequences), a lot of heat is used in the incisions that penetrates into the eye tissues, the Bowman's membrane is severely damaged both by cutting and by thermal fronts.
The idea of the next generation is to cut the lens right inside the cornea, and then get it through a thin incision without this “cap”. The effect is possible because lasers allow focusing inside the tissue, not on its surface. That is, you can make a cut here according to this scheme:
Now we are watching the render operation:
First, the bottom surface of the lens inside the cornea, then the top, then a small incision on the side — and remove the lens with tweezers.
This is what any clinic will show you so that you do not get scared. The real operation looks like this (now telemetry):
First, the patient is asked to look at the flashing green light. The lamp does not just burn, but flashes, so that a person catches it in focus quite often. The eye makes an incredible amount of micro movements, saccades per second, but this is the pace that allows the surgeon to produce a proper eye grip later.

Here you can see the tampon in the defocus (in the video it moves on the left side of the eye) — this surgeon once again wipes the surface to insure against the microbunches of fat floating on it. The second purpose of this touch is to check how the premedication went. The patient must answer if he senses something. He should not feel anything, his nerves are already disconnected with tetracaine.

Here is the capture approaching the eye, which is clearly seen by the appearance closer to the zone of sharpness of the iris:

Alignment and fixation of pneumatic grip is performed. The moment of capture itself can be seen by an easy rotation of the eye, and this effect is very important to control during the correction of astigmatism, because a turn of 30 degrees negates the whole operation for the case of astigmatism. Therefore, the surgeon adjusts the alignment.

After a successful capture, we switch the observation range from visible to infrared to control the process and not blind the patient:

Slowly expanding ring from the edges of the eye to the center is the millions of femtolaser micropulses that form a cut on the upper surface of the lenticular lens inside the cornea. The surface of the cornea is not cut. I recall the main effect — the evaporation of several cells inside the layer of the cornea, and then the release of a relatively large amount of gas, gently pushing tissue.

The bottom surface of the lens is finished:

The second circle, which expands from the center of the eye to the edges, is the upper surface of the lens, which is also cut inside the cornea layer, without direct “piercing” the surface:

At about 01:02 a cut is formed through the surface of the cornea to the cut lens. Lenticule, but in the video it is extremely difficult to make out. Through this incision the lens will reach.
Now, switching the view (and the end of the video from the laser) — the patient from under the control of the CNC is given under the hands of the surgeon (in fact, he moves under the device from under the laser closer to the doctor’s hands). The first step is to wet the eye:

Switching the lens of the microscope, fixing the eye so that it does not twitch, with tweezers. It tucks, but the patient did not feel (for pain relief) and does not even see the tweezers properly (or rather, sees the surgeon's hands above his head):

The incision to extract lentikuly neatly divided instrument — spatula:

This is a very interesting place, the first small spatula First, the upper edge of the lens and the surrounding tissues are separated, and then the lower edge of the lens (in the frame below):

The spatula moves with inconspicuous jerks — this is the resistance of the micro-spikes, arising from the discrete structure of the cut, in some places the individual fibers are not “unstick”, and they need to be moved apart. It’s just not possible to pull the lenticule over the edge, it can catch, so a full spatula is always made on the surface so that air enters the cavity between the upper edge of the lens and the cornea and the lower edge of the lens and the cornea. The most terrible part is as follows:

The surgeon’s hand lies with his elbow on a special support, and with his wrist rests on the patient’s forehead. The spatula is designed so that even if the surgeon is pushed (slightly) or the patient is distracted by a loud bang, the eye will not be damaged. However, all such factors should be strictly excluded.
So, the lens is divided and ready for extraction from the inside of the cornea. The surgeon picks up the tweezers and catches the lenticle:



That's it. You can finish this, but you still need to wash the eyes. Here you can see how the supply of fluid works:

The next stage is the supply of saline directly into the cavity inside the cornea:

As you can see, it will later flow out through the same incision through which the lenticule has been removed. Previously, a second incision was made opposite the first (at the other pole of the eye) to remove this fluid, but it turned out that there was no need for this. Moreover, the smaller the cut, the better.
Smoothing to avoid micro-tabs:

Then — removal of fixing films and the final. You can blink a couple of times. The patient rests for a few seconds, and then slowly gets up and walks into the corridor. In each clinic at the end of the corridor there are hours for control. Next is the dialogue to calm the worrying patient:
“What time is it there?”
— Six minutes past eleven.
— And would you have distinguished the clock from such a distance?
— Oh. For sure.
— Well, everything is in order.
The patient calms down and goes to rest. After 2-3 hours, the eye does not feel anything. You cannot read, write, use a phone or tablet laptop for a day or two to promote fast healing (after all, reading is jogging for the eyes, then you cannot go to a hard sauna or swimming pool for two weeks (until the incision is completely healed to remove lenticules). did not get an infection). That's all.
I hope you have not run away in horror when you saw the spatula. Despite the frightening, I note that this is one of the easiest operations. Gathering the eyes piece by piece after an accident with taking out glass fragments and other side charms on a few hours l bo most precise manual work mikroskalpelem much more difficult and stressful.
On questions of exactly how pneumatic grip works, how you can precisely cut the lens of the desired shape and diameter, what happens to the cornea tissues at the cut border, and why are there such difficulties with cutting the lens inside the eye (and why it is safest). Plus, how the operating room is prepared, how the surgeon soothes the patient, how premedication is performed, what kind of protection there is against unforeseen situations (interruptions in food passing a truck), and so on, I will answer with the next big post. And about the promised comparison of lenses and operations, too, later. All this is a separate topic for discussion, and about them a little later, alas, does not come out much to write. In the first post in the discussion, many topics are superficially affected.